
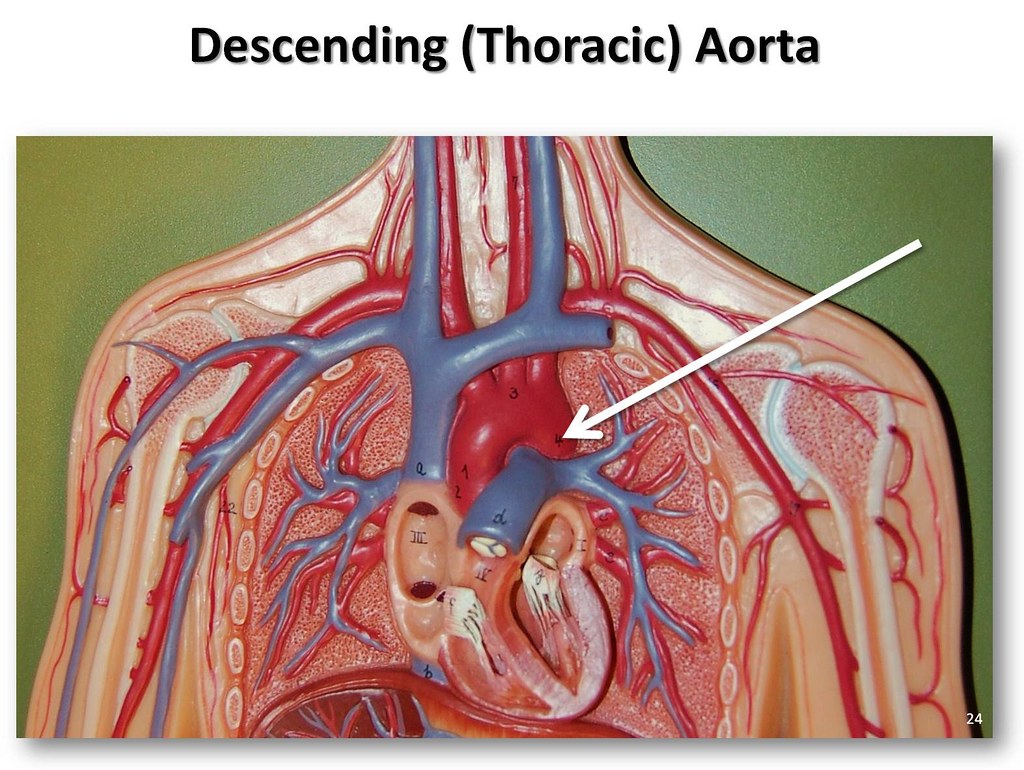
It functions as a peripheral chemoreceptor and is composed of glomus cells.Īn artery originating from the aortic arch.Ī syndrome resulting from structural defects of the arteries that arise from the aortic arch. The portion of the aorta following the aortic arch passing into the chest and abdomen creating the thoracic and abdominal segments.Īn artery arising from the aortic arch that supplies the left arm.Ī small mass that is located in the inferior surface of the aortic arch. (Congential Hypoplasia Aortic Arch, NCI Thesaurus) (Left Common Carotid Artery, NCI Thesaurus)Īn artery arising from the aortic arch that divides into the right common carotid and right subclavian arteries.Īn underdeveloped aortic arch that is present at birth. That being said, HCA alone remains an acceptable approach when arch repair of limited duration (i.e., <30 minutes) is anticipated, and HCA with RCP continues to be favored by some centers because it can remove embolic debris and air, as well as potentially aiding cannulation approaches in cases of acute aortic dissection.An artery arising from the aortic arch that supplies the head and neck. In contemporary practice, nearly all aortic centers have shifted toward routinely using ACP to provide enhanced cerebral protection although such protection may be provided in a unilateral fashion, provided the circle of Willis is complete, many centers, ours included, prefer to provide bilateral protection. Antegrade (ACP) and retrograde (RCP) techniques have been explored, and although definitive data are lacking, ACP appears to substantially reduce operative risk.

Cerebral perfusion (CP) techniques were developed to reduce these risks. Prolonged hypothermic circulatory arrest (HCA) is associated with increased mortality, neurologic morbidity, and other complications. Most aortic arch repairs necessitate a period of systemic circulatory arrest combined with varying degrees of hypothermia to protect the brain and other vital organs. The arch is particularly challenging to repair because-unlike other aortic sections-its replacement usually necessitates interrupting both cerebral and distal aortic perfusion, leaving the brain, spinal cord, and other organs vulnerable. When significant coronary artery disease is identified in an elective surgical candidate, myocardial revascularization is recommended before aortic replacement. Additional investigation may include pulmonary function testing, cardiac stress testing, nuclear imaging, and coronary catheterization. The risk of stroke is significant during aortic arch repair, and because there is a well-known association between aneurysmal aortic disease and carotid artery stenosis, it is useful to perform a screening ultrasound of these arteries. Cannulation strategies may need to be adjusted in patients on the basis of preoperative findings, such as anomalies of branching arch vessels. The diameter of the aorta throughout the diseased and nonaneurysmal portions is determined, and potential sites for cannulation are reviewed for calcification, dissection, and mural thrombus. Common scenarios in which aortic dissection occurs include uncontrolled hypertension, connective tissue disorders (such as Marfan syndrome), and bicuspid aortic valve aortic dissection may cause cerebral malperfusion and result in symptoms such as syncope and neurologic deficits.Įxcept in those patients who require emergent repair, all patients should undergo a thorough preoperative evaluation emphasizing cardiac, pulmonary, and renal function, as well as a careful review of imaging studies.
Arch aneurysms can rupture into the pleural cavity (usually on the left), mediastinum, esophagus, or tracheobronchial tree. New severe pain usually indicates aneurysm rupture or acute dissection. Chest wall compression can cause chronic dull or aching retrosternal or mid-scapular pain. Other problems that can arise from aneurysms involving the aortic arch and the adjacent segments include thromboembolic events such as stroke, and aortic valve regurgitation from associated root enlargement. Patients may have dysphagia from esophageal compression, respiratory symptoms due to airway compression, or edema of the upper body from superior vena caval compression. The onset of symptoms is usually considered an indication of impending rupture or significant malperfusion and should prompt urgent evaluation and repair. When specific symptoms are present, they are usually related to aneurysmal expansion and compression of surrounding structures or to malperfusion related to aortic dissection.


 0 kommentar(er)
0 kommentar(er)
